Appropriate Group A Strep Testing in the Urgent Care Setting: A Quality Improvement Project
Burris A, Jones H, El-Feghaly R, Lee B, Dusin J, Burns A, Linafelter A, Myers A
Children's Mercy Hospitals and Clinics, Overland Park, KS, United States
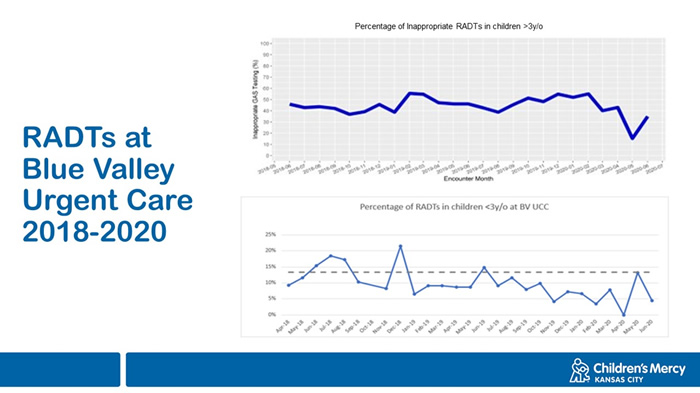
Introduction/Objective: Pharyngitis is one of the most common causes of ambulatory clinic visits; however, group A Streptococcus (GAS) only accounts for 20-30% of cases. Our institution’s clinical practice guidelines recommend against the use of GAS rapid antigen detection testing (RADT) in children <3y/o, and those with viral symptoms. Baseline data review in our urgent care centers (UCCs) and emergency departments from April through September 2018 revealed that 8.8% of RADTs were performed in children <3y/o. A 10% random chart review of the 7678 children >3y/o who had a RADT in that time, found that 44% of RADTs were performed in children with at least 2 viral symptoms or who lacked sore throat. Based on this, we proposed a quality improvement (QI) intervention to decrease the inappropriate use of RADTs in our UCC from 50% to 30% in 2 years.
Methods: A multidisciplinary team convened in September 2018 to evaluate the problems and barriers to change in one of our UCCs. We reviewed institutional, physician and nurse practitioner, and patient factors, identifying countermeasures to institute using Plan-Do-Act-Study (PDSA) cycles. Outcome measures included the number and percentage of RADTS performed on children <3y/o, and the percentage of testing performed on children 3y/o with 2 or more viral symptoms or lacked sore throat. We extracted this information using natural language processing of symptoms recorded in the chart. The process measure was total number of tests. Balancing measures were number of patients tested in repeat visits, and number of parental complaints related to testing. Testing on patients < 3y/o was restricted with prompts in the electronic medical record requiring disclosure of reason for testing prior to the start of this QI project.
Timeline:
PDSA1: December 2018: Sharing initial findings with providers
PDSA2: March 2019: Provider discussion cheat sheet in question and answer format
PDSA 3: July 2019: Family Education posters in rooms
October 2019: Provider Survey
PDSA 4: March 2020: Bulletin board in waiting room. Sharing of data with providers via Microsoft Teams group
May 2020: Presentation for the Family Advisory Council communicating QI goals and data with parents and families
Results: We noted a sustained improvement in inappropriate RADTs in children <3y/o, from a mean of 14% to 5%. Efforts to decrease inappropriate RADTs in children 3 years and older did not have a significant impact, resulting in a mean of 45% with some mild fluctuations.
Conclusions: We saw an improvement in testing of <3y/o following our PDSA cycles, even with the presence of a prompt in the medical record before our interventions. It is unclear why interventions did not have a significant impact on testing of children 3y/o. Continued efforts will focus on impacting provider behavior via individual provider data and further display of our results in our unit.
JOIN OR RENEW WITH SPUC TODAY!
PLAN NOW!
SPUC's 7th Annual Conference
Brought to the learner in virtual format
_____________
Committee Opportunities
Want to make a difference in our developing specialty of Urgent Care Pediatrics?
Join a SPUC Committee or workgroup!
 Winter 2021
Winter 2021

